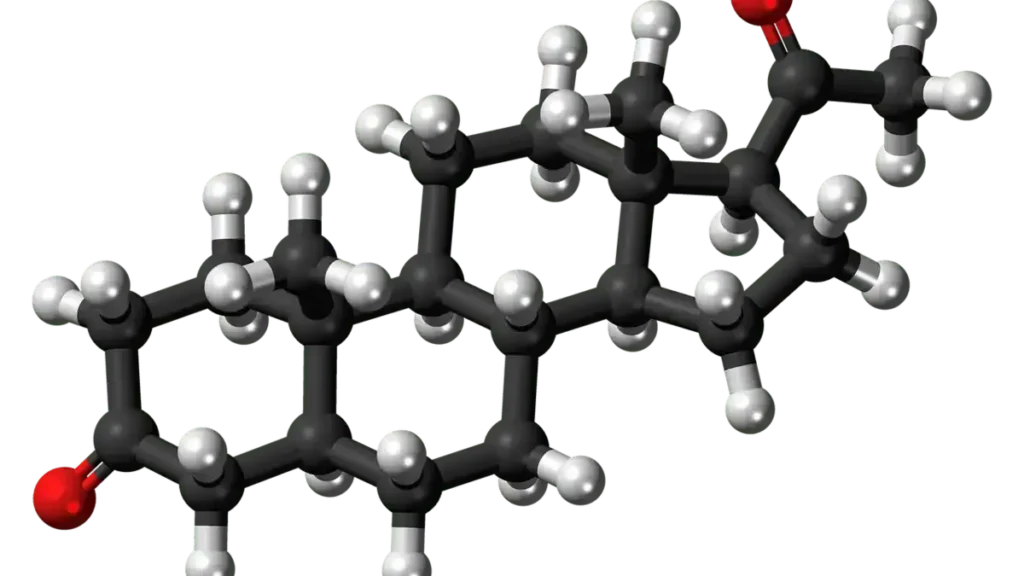
WHAT IS A STEROID?
Steroids, or corticosteroids, are synthetic versions of cortisol, a catabolic endogenous glucocorticoid hormone often referred to as the stress hormone. Cortisol is naturally secreted by the adrenal glands, located on top of the kidneys.
These synthetic hormones mimic cortisol’s powerful effects on the immune system and metabolism, making them essential in treating a wide range of inflammatory and autoimmune diseases.
WHAT IS THE MECHANISM OF ACTION OF STEROIDS?
To understand how steroids raise blood sugar levels, it’s helpful to first know how they work. Their mechanism of action involves immunosuppression and anti-inflammatory activity, as well as significant influence on carbohydrate, protein, and fat metabolism.
By binding to glucocorticoid receptors in almost every cell of the body, steroids regulate the expression of numerous genes. This results in reduced inflammation but also alters metabolic balance, the same pathway that can later contribute to diabetes.
USE OF CORTICOSTEROIDS IN DIFFERENT HEALTH ISSUES
Because of these strong anti-inflammatory effects, corticosteroids such as prednisolone are widely used in conditions like asthma, chronic obstructive pulmonary disease (COPD), multiple sclerosis, and autoimmune disorders such as rheumatoid arthritis.
They are also prescribed for inflammatory skin and gut disorders, including eczema, psoriasis, irritable bowel syndrome (IBS), and hay fever.
However, while they offer rapid relief and disease control, prolonged or high-dose use can bring several unwanted side effects.
SIDE EFFECTS ASSOCIATED WITH STEROID THERAPY
Steroid therapy, though highly effective, is not without risk. Some side effects appear early, while others develop after long term use.
Prominent side effects include hyperglycemia (raised blood sugar), glaucoma, cataracts, mood swings, depression, insomnia, osteoporosis, increased infection risk, and skin thinning.
The likelihood of these effects depends on the dose, duration, and route of administration, for example, oral or systemic forms tend to pose greater risk than topical ones.
HOW STEROIDS CAUSE DIABETES OR HYPERGLYCEMIA
Cortisol plays an important role in maintaining energy balance through its effect on carbohydrate, protein, and fat metabolism. Synthetic corticosteroids imitate these functions but at a more potent level.
Consequently, they can disrupt normal glucose homeostasis and lead to a condition known as steroid induced hyperglycemia or diabetes. Let’s explore how this happens step by step.
1. Enhanced Gluconeogenesis or Increased Hepatic Glucose Production
To begin with, steroids stimulate gluconeogenesis, the process by which the liver produces glucose from non-carbohydrate sources such as amino acids, glycerol, lactate, and pyruvate.
This happens because steroids increase proteolysis (breakdown of muscle proteins) and lipolysis (breakdown of fats), both of which release the substrates required for glucose production.
As a result, more glucose enters the bloodstream, raising blood sugar levels even in the absence of food intake.
Evidence suggests that glucocorticoids increase hepatic enzymes such as phosphoenolpyruvate carboxykinase (PEPCK), intensifying glucose output from the liver.
2. Insulin Resistance by Reducing Cellular Sensitivity to Insulin
In addition to boosting glucose production, steroids reduce how well the body’s cells respond to insulin.
This insulin resistance prevents glucose from being efficiently absorbed by muscle and fat cells. Consequently, glucose accumulates in the bloodstream, leading to hyperglycemia.
This effect becomes more pronounced in people who are already overweight, sedentary, or genetically predisposed to insulin resistance.
3. Hepatic Insulin Resistance (Reduced Liver Sensitivity to Insulin)
Under normal conditions, insulin acts as a signal that tells the liver to stop producing glucose.
However, during steroid therapy, the liver becomes less responsive to insulin and continues releasing glucose even when it’s not needed.
This hepatic insulin resistance is one of the central mechanisms driving sustained high blood sugar during corticosteroid use.
4. High Doses of Steroids Reduce Insulin Secretion
Another key mechanism involves the pancreas. Long term or high dose steroid exposure can impair pancreatic beta-cell function, which means less insulin is secreted.
Without sufficient insulin, glucose cannot move effectively from the bloodstream into the cells, further raising blood sugar levels.
Research published in “Diabetes Care” (2018) confirms that glucocorticoid excess damages beta cells by impairing insulin gene transcription and cell survival.
5. Lipolysis and Its Impact on Insulin Function
Steroids also promote lipolysis, which increases circulating fatty acids. These free fatty acids interfere with insulin signaling pathways and contribute to lipotoxicity, damage to pancreatic beta cells.
This dual action, reduced insulin signaling and beta-cell dysfunction, further worsens hyperglycemia.
WEIGHT GAIN WITH STEROID THERAPY
Another visible and common outcome of steroid therapy is weight gain.
• High doses or prolonged use stimulate appetite by acting on appetite control centers in the hypothalamus. At the same time, disrupted sleep patterns alter hunger-regulating hormones such as ghrelin (which increases appetite) and leptin (which suppresses it).
Moreover, steroids change how the body stores fat, often redistributing it to the face, neck, and abdomen, and cause fluid retention by disturbing electrolyte balance.
Together, these effects make weight management particularly challenging during treatment.
LONG TERM EFFECTS OF STEROIDS ON METABOLIC ACTIVITY
Over time, prolonged or high-dose corticosteroid therapy disrupts the body’s delicate metabolic balance.
• Chronic exposure leads to persistent insulin resistance, chronic hyperglycemia, and a higher likelihood of developing type 2 diabetes mellitus.
• In contrast, short-term therapy may cause temporary hyperglycemia, which usually resolves after discontinuation.
Nevertheless, in individuals who are already prediabetic or obese, even short courses can precipitate long-term metabolic consequences.
CONCLUSION
In summary, steroid therapy is a double-edged sword, highly effective in managing inflammation but potentially dangerous to glucose metabolism.
By increasing gluconeogenesis, reducing insulin sensitivity, and impairing insulin secretion, steroids can trigger steroid-induced hyperglycemia or diabetes.
Therefore, monitoring blood glucose levels regularly, adhering strictly to prescribed doses and duration, and consulting a healthcare professional for any concerning symptoms are essential.
Incorporating healthy lifestyle choices such as balanced nutrition, physical activity, and stress control further reduces risk and supports long-term metabolic health.
FREQUENTLY ASKED QUESTIONS (FAQs)
1. Can steroid-induced diabetes be reversed?
Yes, in many cases it is reversible. If steroids are discontinued or the dose is lowered under medical supervision, blood sugar levels often return to normal. However, prolonged use can cause permanent changes, especially in those with underlying insulin resistance.
2. How soon can blood sugar rise after starting steroids?
Blood glucose can increase within a few hours to days after starting steroid therapy, depending on the dose and individual susceptibility.
3. Are inhaled or topical steroids safer for blood sugar?
Yes. Inhaled and topical steroids act locally and generally have minimal systemic absorption, making them less likely to cause hyperglycemia compared to oral or intravenous forms.
4. Who is at higher risk of steroid induced diabetes?
People with prediabetes, obesity, hypertension, family history of diabetes, or sedentary lifestyle are more vulnerable to developing high blood sugar during corticosteroid use.
5. How can blood sugar be managed during steroid therapy?
Monitoring glucose levels regularly, eating balanced meals, staying active, and following the doctor’s advice regarding dose adjustments or adding antidiabetic medications can help maintain control.
DISCLAIMER
This article is for educational purposes only and does not replace professional medical advice. Always consult your physician, pharmacist, or endocrinologist before starting, adjusting, or stopping any medication, including corticosteroids.
CALL TO ACTION
If you or your loved one is prescribed long term steroid therapy, make blood sugar monitoring a priority. Discuss preventive steps with your healthcare provider to lower the risk of diabetes. Awareness and early management can protect your health and improve treatment outcomes.
Read more: https://pharmahealths.com/metformin-for-dementia-without-diabetes/
REFERENCES
1. Liu D. et al. Diabetes Care. 2018;41(3):e41–e42. “Glucocorticoid-Induced Impairment of Beta-Cell Function.”
2. van Raalte D.H., et al. Lancet Diabetes Endocrinol. 2014;2(9):829–840. “Mechanisms of Glucocorticoid-Induced Insulin Resistance.”
3. Clore J.N., Thurby-Hay L. Endocrine Practice. 2009;15(5):469–474. “Glucocorticoid-Induced Hyperglycemia.”
4. Society for Endocrinology. “Steroid-Induced Diabetes.” 2023 Clinical Guidance.
5. Marik P.E., Varon J. Chest. 2010;137(5):1159–1168. “The Diabetogenic Effects of Stress and Glucocorticoids.”